PATHOPHYSIOLOGY
SLE & Lupus Nephritis: Pathophysiology & Diagnosis
Acknowledgment: Based on GlomCon’s Glomerular Disease Virtual Fellowship seminar “The Guiding Principles for Evaluation of Glomerular Disorders” by Dr. Richard Glassock.
Following an exciting first seminar, the GlomCon fellows learned about the principles governing glomerular disease evaluation. The House of Deposits dived into the literature to find answers to three pertinent related questions:
- What is the burden of glomerular disorders driven by systemic or secondary causes?
- How useful are the tools we have at our disposal for detecting and evaluating glomerular diseases?
- The aim of the game is to preserve kidney function – but do we measure kidney function the right way?
This report takes a closer look at these questions and examines the evidence for common practices.
Following an exciting first seminar, the GlomCon fellows learned about the principles governing glomerular disease evaluation. The House of Deposits dived into the literature to find answers to three pertinent related questions:

Dr. Tanuj Moses Lamech
Nephrology Fellow
Madras Medical College
India
Genetics
- Evidence for a genetic basis:
- 6x increased risk of SLE among first-degree relatives of an index case
- 11-12x increased risk of related autoimmunity (including thyroid disease) among first-degree relatives of an index case
- The risk of SLE among monozygotic twins is 25-50% [risk among dizygotic twins is only 1-2%]
- Monogenic forms of SLE have been identified (genes: DNASE1, TREX1)
- The female predominance of SLE
- Genome-wide association studies (GWAS) have identified several groups of genes associated with systemic lupus
- Genes involving the classical complement pathway (C2, C4, C1q) – highest risk!
- Genes involving interferon regulation and Toll-like receptor (TLR) repression
- Genes involving B cell and dendritic cell function
Environmental Factors
- Ultraviolet light
- Infections: Epstein-Barr virus, parvovirus
- Drugs: hydralazine, isoniazid, procainamide
- Toxins
Pathophysiology of Lupus
Immunological anomalies in lupus:
- High serum levels of Type 1 interferon, overexpression of genes relating to interferon 1
- Increased anergic B cell response
- Increased plasmablast response
- Increased plasmacytoid dendritic cells (PDCs), which are professional antigen-presenting cells
- Widespread antigen presentation overwhelms natural immunological tolerance
- Impaired T-reg function
- Increased low-density neutrophils, which produce neutrophil extracellular traps (NETs)
What is type 1 interferon, and what is the role of TLRs?1
- Toll-like receptors (TLRs) are an evolutionarily ancient system inherited from invertebrates
- They recognize ‘patterns’ from invading viral nucleic acids (often identified by their hypomethylation)
- The recognition of viral nucleic acids sets off a cascade of cytokine signaling, eventually resulting in the production of type 1 interferon (T1 IFN), which is an important anti-viral cytokine
- It aids the transformation of peripheral mononuclear cells into PDCs
- These PDCs produce large amounts of type 1 interferon
- T1 IFN, in turn, can transform other granulocytes into PDCs, thus creating a self-sustaining process
What is an anergic B cell?2
- In the process of V(D)J recombination, an enormous number of B cells with different specificities are generated; some of these cells, however, are autoreactive
- One of the ways in which the body’s natural tolerance mechanisms deal with such autoreactive B cells is to render them irresponsive (‘anergic’) to antigenic stimulation
- Such anergic B cells remain in circulation but have a much shorter lifespan and are eventually culled
- However, in the presence of very high levels of B-cell activating factor (BAFF), as occurs in lupus, such anergic B cells can survive and generate auto-antibodies
A Unified Theory for the Development of Systemic Lupus
- DNA/RNA release occurs in response to normal cellular injury, viral infections, environmental factors such as UV light, or increased production of NETs
- The mechanisms by which such DNA/RNA lead to autoimmunity include:
- Abnormalities in the metabolic pathways that clear DNA/RNA, resulting in accumulation of nucleic acids and likely stimulation of TLR-mediated interferon production
- Associated with Mendelian forms of lupus
- Abnormalities in complement-mediated opsonization of apoptotic debris (including DNA/RNA), preventing clearance
- Genetic variants increase the risk of lupus 5-10-fold
- Recognition of human DNA by TLRs due to abnormalities in genes that normally repress their activity
- Genetic variants increase the risk of lupus 1.3-1.4-fold
- Increased production of type 1 interferon via TLR signaling due to irregularities in genes that regulate type 1 interferon
- Genetic variants increase the risk of lupus 1.2-1.3-fold
- Increased production of autoantibodies due to defects in T cell and B cell function
- Genetic variants increase the risk of lupus 1.1-1.2-fold
- Abnormalities in the metabolic pathways that clear DNA/RNA, resulting in accumulation of nucleic acids and likely stimulation of TLR-mediated interferon production
- Thus, there appears to be a step-wise hierarchy of risk influencing the eventual development of lupus
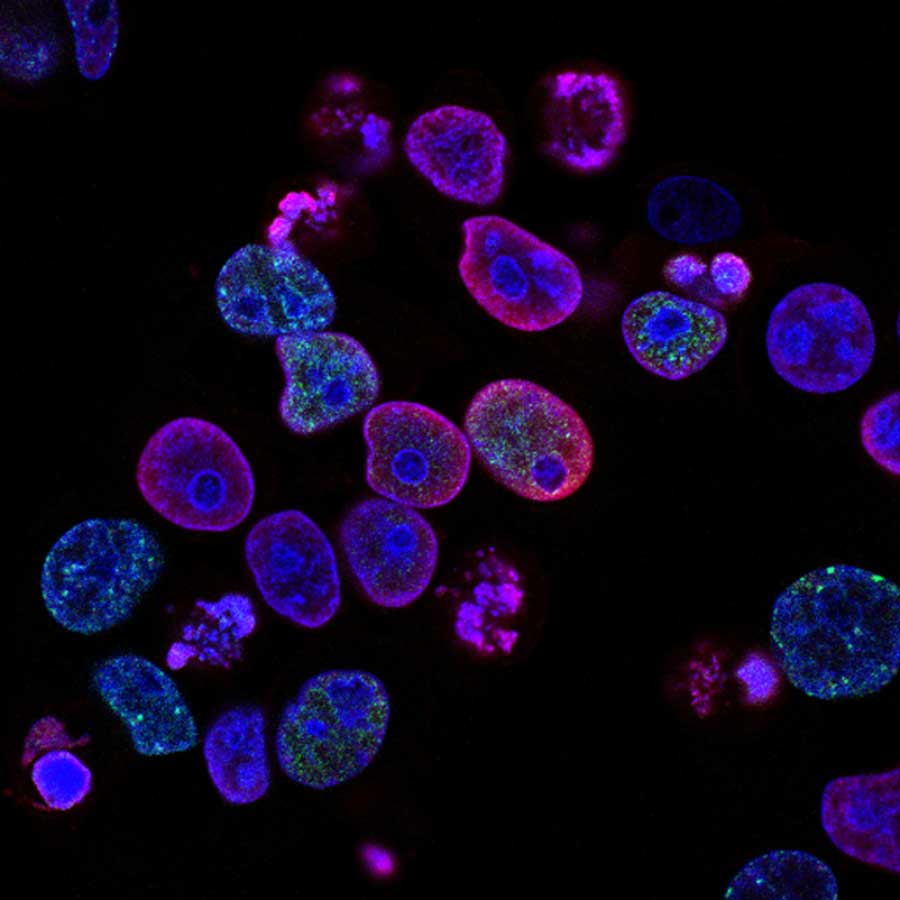
Pathophysiology of Lupus Nephritis
- The critical step in lupus nephritis is the occurrence of antigen-antibody complexes in the kidney
- Previously, it was thought that autoantibodies bind to circulating antigens, and these then deposit in the kidney
- Recently, it has been demonstrated that antibodies may form at tertiary lymphoid tissues within the kidney itself3
- Antibodies can deposit onto nuclear antigens that have become trapped in the kidney
- These antigen-antibody complexes then set off an inflammatory cascade, which recruits neutrophils
- These neutrophils produce inflammatory cytokines, apoptosis, and make NETs, resulting in further antigen exposure within the kidney
Serology
- CRP is a complement protein and therefore does not correlate well with lupus activity
- ESR reflects an inflammatory state and correlates better with lupus activity
- ANAs
- Initially thought to occur in 98% of cases at presentation
- True prevalence closer to 85%, with detection sometimes requiring serial ANAs to be done over some time
- Thus, though ANA-negative lupus is unusual, it should not exclude the diagnosis
- Titres of 1:80 or less are seen in 5% of the general population
- Therefore, only high titers, in the range of 1:240, should be considered to have clinical significance
- dsDNA
- Highly specific and associated with lupus nephritis
- dsDNA has a high negative predictive value and a low positive predictive value
- dsDNA may be detected by Crithidia luciliae indirect fluorescence assay or by ELISA
- Crithidia assay is more specific
- ELISA sometimes detects low-affinity dsDNA that is not pathogenic
- C1q antibodies
- Associated with proliferative LN and may be pathogenic
- C3, C4
- At a population level, the reliability of C3 and C4 for tracking disease activity is poor
- The membrane attack complex (C5b-9) tracks best with lupus nephritis but is currently limited to the research environment
- Anti-Smith antibody
- When present, it is strongly predictive of lupus
- However, it cannot be used to monitor disease activity
- Urinary biomarkers in lupus (APRIL, BAFF) are currently of limited utility
References
1. Crow MK. Type I Interferon in the Pathogenesis of Lupus. J. Immunol. 192, 5459–5468 (2014). [https://www.jimmunol.org/content/192/12/5459]
2. Isnardi I, Ng YS, Menard L, Meyers G, Saadoun D, et al. Complement receptor 2/CD21− naive human B cells contain mostly autoreactive unresponsive clones. Blood 115, 5026–5036 (2010). [https://ashpublications.org/blood/article/115/24/5026/27217/Complement-receptor-2-CD21-human-naive-B-cells]
3. Robson KJ, Kitching AR. Tertiary lymphoid tissue in kidneys: understanding local immunity and inflammation. Kidney Int. 98, 280–283 (2020). [https://www.kidney-international.org/article/S0085-2538(20)30504-4/fulltext]
