DISEASE OUTCOME
Lupus Nephritis: Predictors of Outcome
Acknowledgment: Based on GlomCon’s Glomerular Disease Virtual Fellowship workshop on lupus nephritis by Dr. Tingting Li.

Dr. Diana Mahbod
Nephrologist
Dallas Renal Group
USA
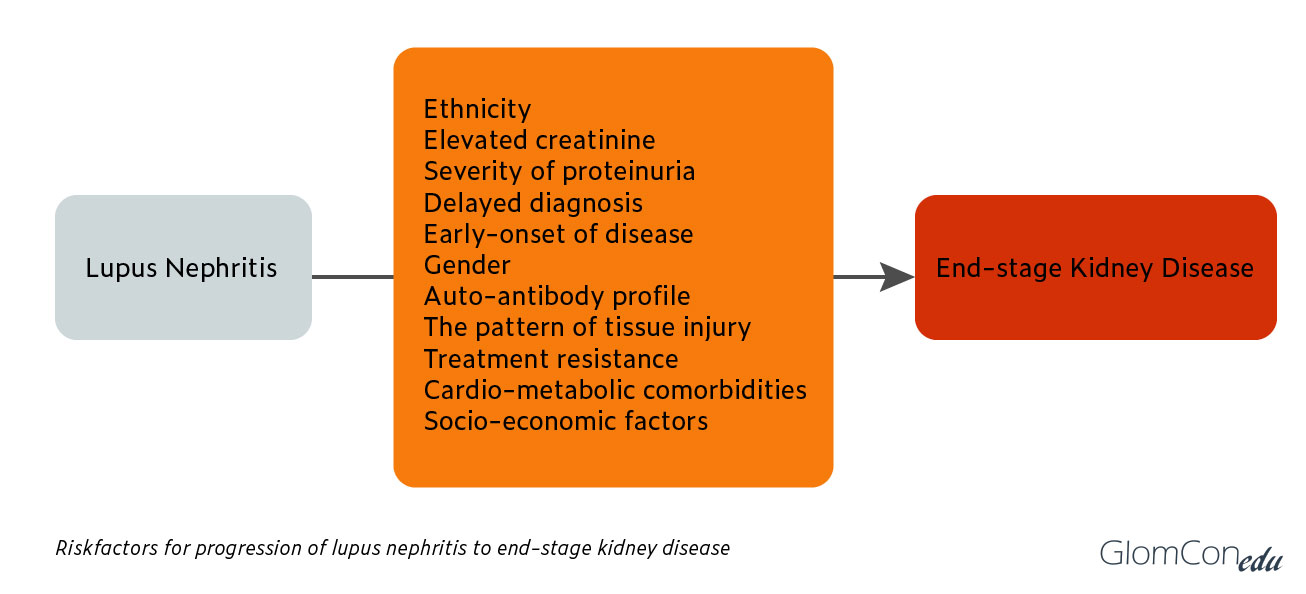
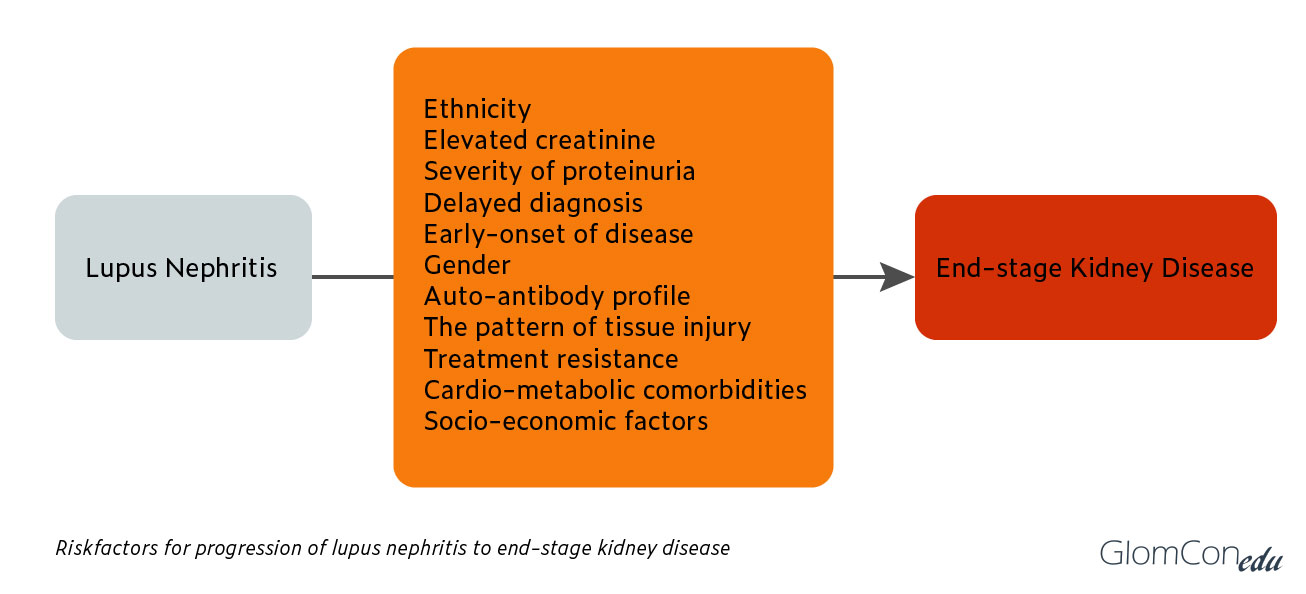
What are predictors of ESRD in Lupus Nephritis?
Lupus nephritis (LN) occurs in up to 60% of adults and 80% of children with SLE1
- Renal disease in SLE is clinically variable2
- can range from “silent” nephritis to RPGN to nephrotic syndrome, or a combination
- can occur in various forms during a patient’s lifetime
- 10-30% of patients with LN develop ESRD within 15 years
- Patients with SLE develop ESRD at a relatively young age3
- 73% of SLE patients with ESRD are <50 years old
- The average age of ESRD onset in LN is 41 years old
- Renal damage is a significant predictor of mortality in patients with SLE4
Treatment of LN has changed significantly since the 1960s, resulting in improvement in outcomes3.
- identification of histologic subtypes based on biopsy
- demonstration of adequate immunosuppression to treat LN
- improvement in survival rate from <50% in the 1960s to 80% in the 1990s
Risk factors for progression to ESRD include demographic, clinical, and socioeconomic factors5
| Factors that may influence the presentation or prognosis of Lupus Nephritis (adapted from Ntatski & Isenberg, 2015) |
|---|
Demographical
|
Environmental
|
Genetic
|
| Hormonal |
Immunological
|
Histology
|
Clinical & Laboratory Markers
|
Therapy
|
Some key points:
Age
- renal disease is more frequent and severe in childhood than adult-onset SLE
- younger age at nephritis onset is a poor prognostic indicator in adults
- late-onset SLE (>50 years old) is associated with fewer major organ manifestations
Sex
- men with SLE have more frequent and severe LN than females
- area for further study: is this biological (such as related to hormones) OR is it due to delay in diagnosis, the difference in healthcare-seeking behavior, and treatment compliance?
Ethnicity
- Black and Hispanic patients have been found to have higher rates of renal disease and mortality
- area for further study: the role of biology/genetics (such as APOL1, see below) vs. socioeconomic and sociocultural factors (remains controversial)
Environmental/socioeconomic
- Socioeconomic status is complex and challenging to measure6
- Patients with private insurance were found to have a later onset of ESRD (by eight years!) compared to no insurance OR Medicaid7
Genetic
- Genetic associations have been found for the development of SLE
- One association for the development of renal disease in SLE: FCGR genes
- family of immunoglobulin Fc receptor genes found on many immune response cells
- strong association with end-organ damage, including ESRD
- PROFILE cohort – multi-center, multi-ethnic, started in 1998
- FCGR3A*GG overrepresented in patients who developed ESRD8
- APOL1 polymorphisms are associated with risk of LN-ESRD and time to progression to ESRD in African Americans9
Immunologic
- immune complexes formed in the circulation can deposit in glomeruli and lead to complement activation and inflammation
- anti-dsDNA is linked to proliferative LN, and rising titers may be predictive of proliferative LN occurrence, but studies have not shown an association with interstitial fibrosis and tubular atrophy (IFTA) or progression to ESRD10
- area for further study: anti-C1q also strongly correlated with renal involvement, but value as a prognostic marker requires further study
- area for further study: does anti-phospholipid antibody cause glomerular and capillary thrombosis, chronic vasculopathy, associated arterial hypertension, and thus negatively impact renal survival?
Histopathology
- Worse renal outcomes:
- Class 3 or 4 LN2
- Chronicity on index biopsy, seen as tubulointerstitial damage (TID), or IFTA11
- Moderate-to-severe TID was seen in 13% of SLE patients with eGFR>60 mL/min, 33% of SLE patients with eGFR 30-60 mL/min
- area for further study: role of protocol biopsies?
- Moderate-to-severe TID was seen in 13% of SLE patients with eGFR>60 mL/min, 33% of SLE patients with eGFR 30-60 mL/min
Tang, et al. created a tool to predict the risk of renal disease progression, to use detailed pathologic lesion score over pathologic subtype12
| Variables | Scores |
|---|---|
| Cellular crescents | 1, 3, or 5 points |
| Fibrous crescents | 1-3 points |
| Active index >20 | 7 points |
| Chronic index >5 | 5 points |
| Glomerular sclerosis | 1 or 3 points |
| Interstitial fibrosis | 1, 2, or 4 points |
| Nephrotic syndrome | 2 points |
| eGFR<45 mL/min | 6 points |
Serum complement levels may predict worse outcomes, but C1q and C3 deposits on biopsy did NOT predict ESRD or death in patients with SLE13
This figure adapted from a review article by Maroz and Segal4 summarizes it well:
References
- Lupus 1999; 8(4): 287-292
- Lupus 2005; 14(1): 39-44
- Arthritis Rheum 2011; 63: 1681-8
- Am J Med Sci. 2013; 364(4): 319-23
- Expert Review of Clinical Immunology 2015;11:837-848
- Rheumatology 2006; 45: 1144-1147
- Journal of Rheumatology 2007; 34:10
- PLoS Med 2006; 3(10): e396
- Arthritis & Rheumatology 2014; 66(2): 390-396
- Semin Arthritis Rheum. 2019; 49(3): 396-404
- Semin Arthritis Rheum. 2018; 47(4): 545-551
- Medicine 2017; 96: 37
- Rheumatology 2020; 0:1-8

Excellent summary. Many thanks. Waqar