GLOMERULAR DISEASE MANAGEMENT
Alport Syndrome: Clinical Presentation, Natural History, and Management
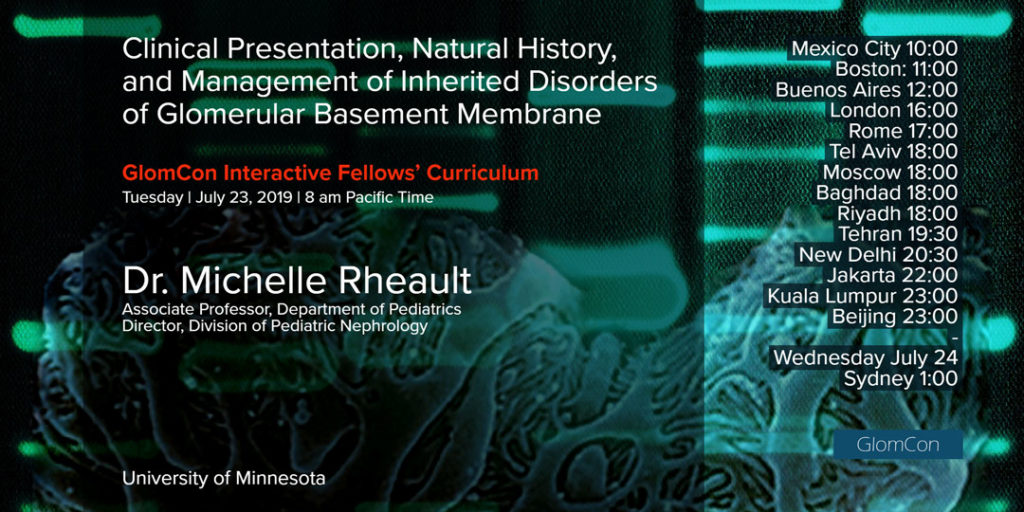
Dr. Michelle Rheault, Associate Professor, Department of Pediatrics, and Director of the Division of Pediatric Nephrology, University of Minnesota Medical School, reviewed the natural history and clinical management of Alport syndrome. Our Moderator’s Notes are derived from her live presentation.

By Dr. Kate Robson
Genetics
Alport syndrome is a hereditary disorder of basement membranes caused by mutations in COL4A3, COL4A4, COL4A5 genes (encoding alpha chains of type IV collagen).
Type IV collagen is a major component of basement membranes. Alpha 3, 4 and 5 chains form triple helices, which are bound together to form a network in the glomerular basement membrane (GBM).
Milder (e.g. missense) mutations result in abnormal triple helix formation and faulty networks. When mutations are severe (e.g. deletions, stop codons), the corresponding alpha chain is not produced and the triple helix cannot form at all. The other alpha chains are subsequently degraded and the network is not made.
| Gene | Encodes | Chromosome | Mutations associated with |
|---|---|---|---|
| COL4A3 | Alpha 3 | X chromosome | X-linked Alport syndrome (AS) |
| COL4A4 | Alpha 4 | Chromosome 2 | Autosomal recessive or dominant AS |
| COL4A5 | Alpha 5 | Chromosome 2 | Autosomal recessive or dominant AS |
Clinical Features
Classic clinical features include:
- hematuria and proteinuria with progressive chronic kidney disease
- microscopic +/- gross hematuria initially
- progressive development of proteinuria
- declining glomerular filtration rate (GFR)
- sensorineural hearing loss (abnormal cochlear basement membrane)
- usually bilateral
- high frequency loss first
- not congenital (newborn hearing screen normal; hearing loss starts from approx. 5 years old)
- ocular abnormalities
- lens capsule thinning
- anterior lenticonus
- recurrent corneal erosions
- maculopathy (does not affect vision but is diagnostic of Alport syndrome)
These manifestations are variable dependent on the individual’s genetic status.
Epidemiology
Alport syndrome affects approximately 1 in 50,000 people. It accounts for 1.3% (children) and 0.4% (adults) of end-stage kidney disease in the USA.
Data from tertiary studies indicates that Alport syndrome is diagnosed in 12-27% of children presenting with persistent microscopic hematuria.
Traditionally, it is understood that X-linked disease accounts for the majority (˜80%) of Alport syndrome, autosomal recessive contributes ˜15% and autosomal dominant Alport syndrome is rare (<5%). More recent next-generation sequencing data suggests that autosomal dominant Alport syndrome is more common (19-31%).
Pathological findings
Light microscopy shows nonspecific changes only, such as interstitial fibrosis and tubular atrophy, or focal segmental glomerulosclerosis (FSGS) pattern (predominantly seen with mutations in COL4A3 & COL4A4).
Immunofluorescence for type IV collagen alpha chains is helpful.
Electron microscopy is essential to the diagnosis. Early in the disease course, thinning of the GBM may be the only finding.
Other features emerging later are:
- irregular, thickened GBM
- ‘basket-weaving’ lamellations in GBM
- podocyte effacement
(for a more detailed review of the histopathology of Alport syndrome, watch the GlomCon session by Dr. Dominick Santoriello https://glomcon.org/genetic-causes-of-gn/the-pathology-of-genetic-causes-of-glomerular-kidney-disease/)
Natural History
X-linked Alport syndrome (Males)
50% of males with X-linked Alport syndrome develop ESKD by age 25, 80% by age 40 and 100% by age 60. Severity of mutation is correlated with rate of progression.
X-linked Alport syndrome (Females)
Females with X-linked Alport syndrome (previously considered unaffected ‘carriers’) are now recognised to be at risk due to X chromosome inactivation (mosaicism). By age 40, 50% have proteinuria and 12% have ESKD [Jais et al 2003, Rheault et al 2016]. Disease course is variable, and correlates neither with mutation severity nor with the disease course in male relatives. Skewing of X inactivation may influence disease severity, and other modifier genes may also have an impact.
Autosomal recessive Alport syndrome
Limited data suggests that disease course in autosomal recessive Alport syndrome is similar to that seen in males with X-linked Alport syndrome, with 50% developing ESKD by mid-20s [Oka et al 2014].
Autosomal dominant Alport syndrome
Recent data indicates these patients have a more slowly progressive course, with median proteinuria development at 17 years old, and median renal survival of 70 years [Kamiyoshi et al 2016].
Treatment
There are no specific treatments currently available for Alport syndrome. Early ACE inhibitor therapy has been shown to delay ESKD in a registry-based study of sibling pairs [Gross et al 2012].
Consensus guidelines currently recommend ACE inhibitor treatment for patients (male & female) with proteinuria, but not for those with isolated hematuria. Patients with microalbuminuria and hematuria may benefit depending on the severity of mutation and family history. The ‘EARLY PRO-TECT’ clinical trial is currently investigating ramipril vs placebo in this group [see References].
Practice Points
- ‘Thin basement membrane’ and ‘benign familial hematuria’ are not diagnoses: characterise a diagnosis based on clinical and genetic criteria [Kashtan et al 2018]
- Genetic testing can precede or replace kidney biopsy depending on patient’s age, clinical setting, and family history
- Detailed family history of kidney, hearing and vision problems is important
- Consider other family members at risk when making a new diagnosis
- A patient diagnosed with ‘FSGS’ may have Alport syndrome
- Post-transplant anti-GBM disease can affect patients with Alport syndrome, most commonly those with complete absence of type IV collagen chains.
- Patients in Canada and USA can enrol in Alport Syndrome Treatment and Outcomes Registry (ASTOR) at www.alportregistry.org
References
Jais et al 2003: https://www.ncbi.nlm.nih.gov/pubmed/14514738
Oka et al 2014: https://www.ncbi.nlm.nih.gov/pubmed/24633401
Kamiyoshi et al 2016: https://www.ncbi.nlm.nih.gov/pubmed/27281700
Gross et al 2012: https://www.ncbi.nlm.nih.gov/pubmed/22166847
EARLY PRO-TECT: https://www.ncbi.nlm.nih.gov/pubmed/22811928
Kashtan et al 2013: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3505543/
Kashtan et al 2018: https://www.ncbi.nlm.nih.gov/pubmed/29551517 1
Rheault et al, Females with X-linked Alport syndrome are under-diagnosed and under-treated, Pediatric Academic Society Abstract 2016.

Dear Kate,
I noticed in this pubs that the COL4A3 gene is reported to be on the X chromosome and the COL4A5 gene on the Chromosome 2. I believe this should be the opposite, COL4A3 gene is localized on the chromosome 2 together with COL4A4, while the COL4A5 gene is located on Chromosome X.
Kind regards,
Magali
Excellent write up