MINI-REVIEW
Anticoagulant-related nephropathy
Authors
Irene Martin1, Paolo Nikolai So2, Tiffany Caza3, Mohamed Hassanein4
Affiliation
1 Hospital Universitario 12 de Octubre, Madrid, Spain
2 Piedmont Athens Regional Medical Center, Georgia, USA
3 Arkana Labs, Arkansas, USA
4 University of Mississippi Medical Center, Mississippi, USA
Introduction and epidemiology
Anticoagulant-related nephropathy (ARN) was first described a decade ago when Brodsky et al. found, in a retrospective analysis of 2801 biopsies, 9 cases of hematuria and acute kidney injury (AKI) in patients with supratherapeutic levels of warfarin. Thus, it was first named warfarin-related nephropathy (WRN). With the emergence of the novel oral anticoagulant (DOAC), new cases of ARN have been described in patients treated with dabigatran, apixaban and rivaroxaban. In a retrospective analysis, a 37% prevalence of ARN has been described in patients treated with warfarin. DOAC related nephropathy has been less studied, although dabigatran has been associated with a higher prevalence of kidney related side effects with a 4.6% prevalence, while rivaroxaban, apixaban and edoxaban were associated with 3.5%, 2% and 1.7% respectively. Nevertheless, ARN might be underdiagnosed because in most instances, nephrologists exhibit hesitancy to conduct kidney biopsies in patients requiring therapeutic anticoagulation. This reluctance is due to the potential thrombosis/thromboembolism risk during the suspension of systemic anticoagulation and the likelihood of hemorrhage occurring at the kidney biopsy site after the resumption of systemic anticoagulants.
Pathogenesis
Although the pathogenesis of ARN is still not well understood, it has been proposed that, in addition to treatment with oral anticoagulants, some additional risk factors predisposing to the development of hematuria and AKI should be present. The reason is that when analyzing patients on warfarin treatment, the mean INR did not differ between those who developed ARN and those who did not. The main risk factors are the pre-existence of a glomerular disease involving the glomerular basement membrane, such as thin membrane, IgA nephropathy, lupus nephritis, etc., or a condition that produces a glomerular hyperfiltration, for instance, chronic kidney disease, diabetes mellitus, hypertension, obesity, etc. These conditions facilitate the migration of red blood cells through the glomerular filter, which, under normal conditions, is about one red blood cell per 109 erythrocytes passing through the glomerulus every 24 hours. The presence of massive hematuria in the renal tubules could lead to AKI due to tubular obstruction, although the absence of Tamm-Horsfall protein questions this theory.
In addition, the release of heme group from the hemoglobin contributes to tubular damage through the release of reactive oxygen species (ROS), the activation of the alternative complement pathway and activation of various inflammatory pathways. Thus, tubular cell death and apoptosis are induced.
The level of INR required to induce ARN is not well defined. In some cases, ARN has been associated with INR levels above 4, whereas in others, ARN was present once the coagulopathy resolved.
Clinical Presentation
Most patients present with macroscopic hematuria and AKI. Patients with severe AKI often develop hypertension, excessive fluid retention and low urine output. In the majority of individuals with ARN, the serum creatinine levels tend to stabilize or show a modest improvement during the initial weeks after rectifying the effects of warfarin coagulopathy. The time to resolution of hematuria and normalization of serum creatinine and INR is not well-defined in the literature, however, in most studies when renal function improves, it typically does so within the first 3 months, with a low likelihood of further improvement beyond that period. Nevertheless, a significant portion of these patients may experience minimal to no recovery of their kidney function. In a study that included 45 patients with biopsy-proven ARN, only 37% showed improvement in renal function. When hematuria persists despite these interventions, it suggests the potential presence of an underlying glomerulonephritis or abnormalities in the thickness of the glomerular basement membrane.
The differential diagnosis of this pathology includes those conditions that present with AKI and hematuria. It is essential to rule out a urological condition of hematuria, such as nephroureteral lithiasis or urinary tract tumors. Urine sediment will help us to identify dysmorphic red blood cells that point to a glomerular condition. Among the glomerular conditions, IgA nephropathy and renal vasculitis are the most common causes.
Histology
The diagnosis of this pathology is eminently clinical. However, the performance of kidney biopsy helps in cases in which multiple comorbidities coexist. The biopsy of these patients showed most of the changes in the tubulointerstitial space with innumerable red blood cells, some of them dysmorphic, obstructing the tubular lumen and the Bowman’s space (Figure 1). The peculiarity of these casts was that most of them were located in the distal tubules, and therefore in the medulla, and that they did not contain Tamm-Horsfall protein. By contrast, the glomeruli showed no changes, although in some cases they revealed an underlying glomerular pathology, such as an IgA nephropathy, a thin glomerular basement membrane, mild lupus nephritis or focal and segmental glomerulosclerosis (FSGS) pattern of injury. In addition, the Perls’ Prussian Blue tinction can identify heme-containing molecules and free iron.
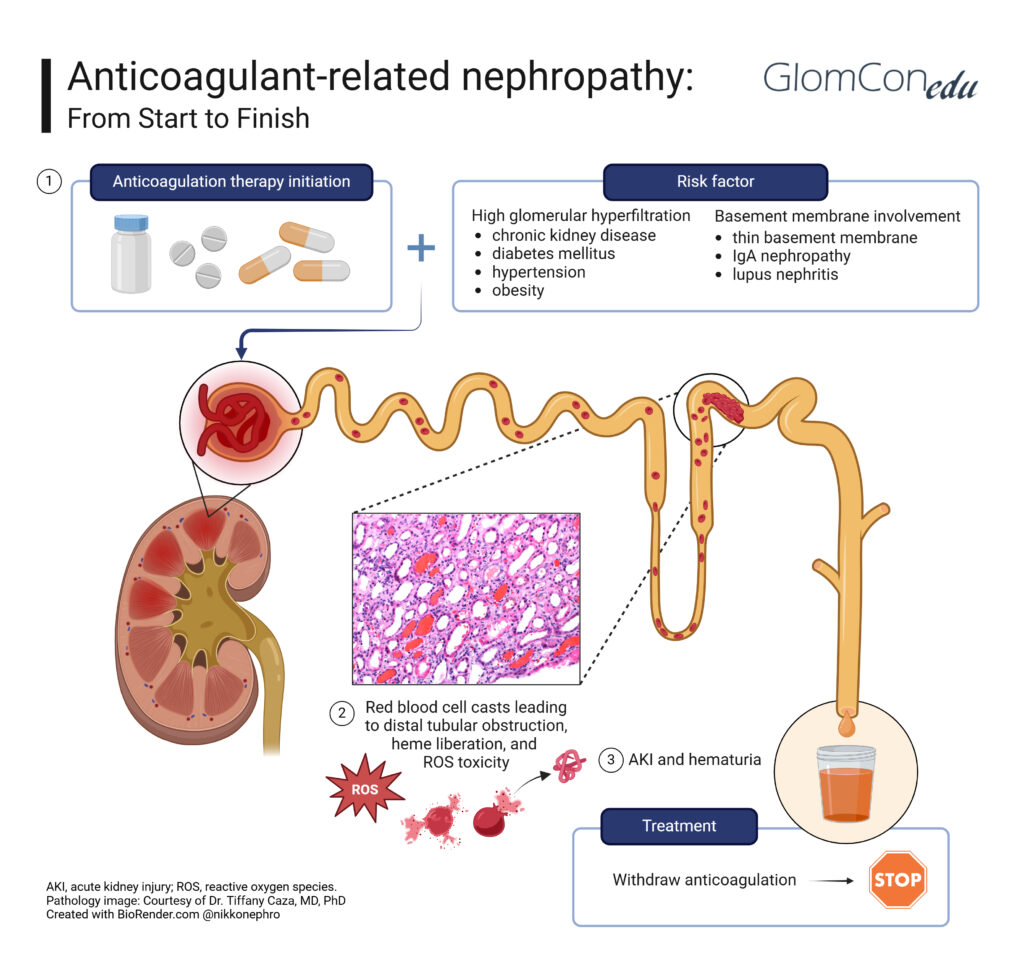
Figure 1. Pathogenesis and management of anticoagulant-related nephropathy
Treatment
ARN treatment is mainly supportive and should start with the withdrawal of anticoagulants. Futhermore, steroids have been proposed as a possible treatment in ARN. In a study published by TB Mikic et al. eight patients were treated with methylprednisolone after diagnosis of ARN for 6 to 8 weeks with improvement of renal function. However, the recommendation of steroid therapy is still limited to a few reported cases, and probably, to the positive experience of some centers of the use of corticosteroids in acute renal failure with macroscopic hematuria of IgA nephropathy.
On the other hand, hemodialysis can be useful as a supportive treatment in cases of severe renal failure. Although it could be considered as a treatment to remove an excess dose of oral anticoagulants, its effectiveness is generally limited due to the protein binding of these drugs. An alternative is the use of anticoagulant reversal agents if available (e.g., vitamin K for warfarin, idarucizumab for dabigatran).
Given the high proportion of patients treated with oral anticoagulants, ARN prevention has become a priority. Thus, kidney function monitoring and careful INR titration is essential, especially in the first 3 months, since it has been shown that the risk of ARN is higher in the first 6-8 weeks after initiation of anticoagulation.
Conclusion
In summary, ARN is indeed a genuine condition, but the scarcity of histologic confirmation results in a lack of information on its incidence, prevalence and pathophysiology. The specific cause of ARN remains unclear, it could be a consequence of red blood cells in glomeruli and renal tubules, with iron release from erythrocytes, or direct toxicity on renal cells and microvasculature. In the management of ARN, strict monitoring of anticoagulation is necessary, especially in patients with various comorbidities or risk factors for its development and avoidance of excessive anticoagulation.
