GLOMERULAR DISEASE DIAGNOSIS
Antiphospholipid Syndrome
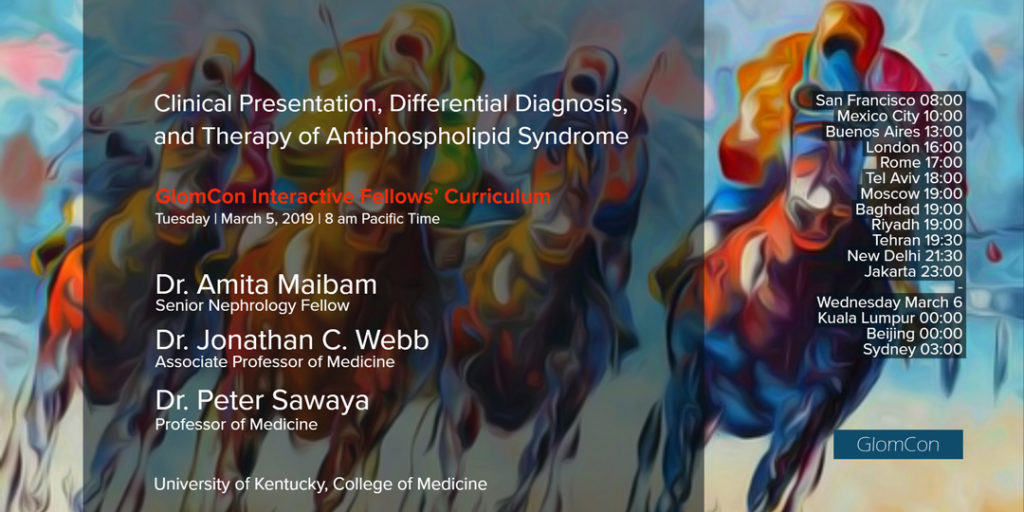
A GlomCon Conference led by Drs. Maibam, Sawaya & Webb from the University of Kentucky. Our Moderator’s Notes are derived from their live presentation.

By Dr. Michelle O’Shaughnessy
Key points:
- Antiphospholipid syndrome (APS) is a systemic autoimmune disease defined by the presence of venous or arterial thrombosis and/or adverse pregnancy outcomes PLUS persistent (on ≥ 2 occasions at least 12 weeks apart) antiphospholipid (aPL) antibodies (anti-cardiolipin, anti-beta-2-glycoprotein-I, or positive lupus anticoagulant activity).
- Renal (thrombotic microangiopathy = TMA, venous/arterial thrombosis), hematologic (hemolytic anemia, thrombocytopenia), cardiac (valvular vegetations/thickening), dermatologic (livedo reticularis), and neurologic (stroke, cognitive impairment) manifestations are observed.
- Pathogenesis is not fully understood, but aPL antibodies appear to activate complement, inflammatory cells, and endothelial cells through a number of pathways, ultimately promoting coagulation and interfering with trophoblasts and decidual cells.
- Kidney biopsy findings include: thrombi within the glomerular capillaries; capillary congestion; mesangiolysis (apoptosis of mesangial cells); fibrinoid necrosis of the afferent arteriole; collapsed (ischemic) capillary loops; and (by EM) subendothelial electron lucent material. Over time, double contouring of the basement membrane (MPGN pattern of injury) without immune deposits can develop.
- Differential diagnosis for renal TMA includes: autoimmune disorders (APS, SLE, systemic sclerosis); severe hypertension; severe preeclampsia, eclampsia, or HELLP syndrome; systemic infection or cancer; or following hematopoietic stem cell or organ transplantation.
- Catastrophic APS (CAPS) requires all 4 criteria to be met for a definite diagnosis: 1) involvement of 3 or more organs, systems or tissues; 2) simultaneous appearance of manifestations within <1 week; 3) small vessel occlusion in at least one organ or tissue confirmed by histopathology; 4) laboratory confirmation of the presence of aPL antibodies.
- Treatment involves anticoagulation and immunosuppression.
- Anticoagulation (life-long, for all patients with APS): Warfarin appears more effective than rivaroxaban (Pengo et al, Blood 2018), and a target INR of 2-3 is as effective, and safer, than a higher target of 3-4.5 (Finazzi et al, J Thromb Haemost. 2005).
- Immunosuppression (for patients with CAPS): Corticosteroids and therapeutic plasma exchange are standard of care for CAPS (although RCTs lacking). IVIG, rituximab, eculizumab, and defibrotide can be considered in refractory cases (Cervera et al, J Autoimmun 2009).
- ESRD populations:
- HD: There is an increased risk for AV graft (but not fistula) thrombosis, and warfarin might reduce this risk (RCTs lacking)
- Transplant: In those with a history of APS, warfarin or sirolimus might reduce the risk for intrarenal or systemic clotting events (RCTs lacking)
