DIAGNOSTIC WORKUP
Kidney Biopsy – A Brief Report
Acknowledgment: Based on GlomCon’s Glomerular Disease Virtual Fellowship workshop on the basics of kidney biopsy evaluation by Dr. Vivek Charu. At this workshop, GlomCon fellows discussed the basics of a kidney biopsy.

By Dr. Anju Mohan
Nephrology Fellow
University of Chicago
USA
Techniques:
- Currently, percutaneous aspiration needle biopsy using a spring-loaded automated cutting needle biopsy “gun” is used for kidney biopsy. The preferred position for native kidney biopsy is prone, with lateral decubitus being an alternative option; for transplant biopsies, the preferred position is supine. A prebiopsy ultrasound is performed to identify the optimal biopsy site: the lower pole of the native left kidney and the most easily accessible pole of the transplant kidney is typically preferred. In most centers, the biopsy procedure itself is also guided by real-time ultrasound or CT imaging.
- The procedure entails the following – After local anesthesia, the skin is lanced, and the biopsy needle is inserted and advanced until the tip reaches the outer cortex. The biopsy gun is then activated.
- 14-16 gauge needles in adults and 16-18 gauge needle in kids are preferred to optimize diagnostic yield. Usually, 2-3 attempts are made with a maximum of 5 passes. Institutional variations are present.
- Other techniques infrequently used are the transjugular retrograde approach, laparoscopic technique.
Complications:1
- Generally, the procedure is safe.
- Hematuria – 35 %
- Perinephric hematoma (usually not requiring any intervention) – 65%
- Transfusion < 1% of biopsies
- Renal loss <0.1% of cases
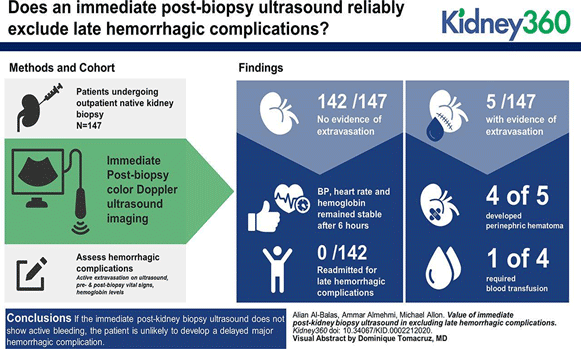
Is a repeat kidney US immediately after biopsy helpful?
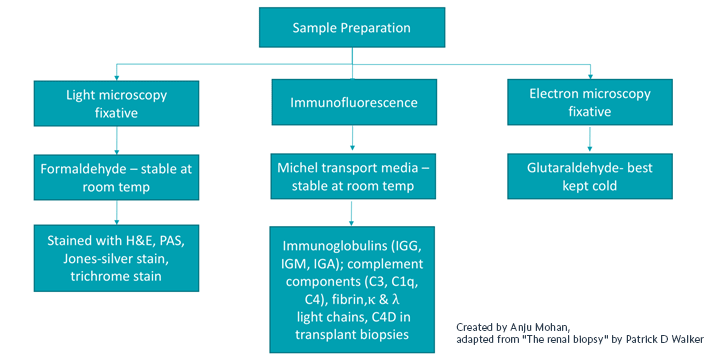
Sample preparation:
Ideally, a renal pathologist should evaluate the tissue using a dissecting microscope to confirm that glomeruli are present in real-time during the procedure, but this is not available at all the centers. After that, the tissue cores are divided into three samples (most typically of roughly equal size) and placed in appropriate transport media or fixatives for light, immunofluorescence, and electron microscopy.
The kidney biopsy report:
- Clear communication between the nephrologist and the renal pathologist is key as clinicopathological correlation is generally required to make the correct, pathophysiologically driven diagnosis.
- Usually, the pathology report entails:
- Brief gross description
- LM, IF/IH, EM findings on:
- Glomeruli
- Tubules
- Blood vessels
- Interstitium
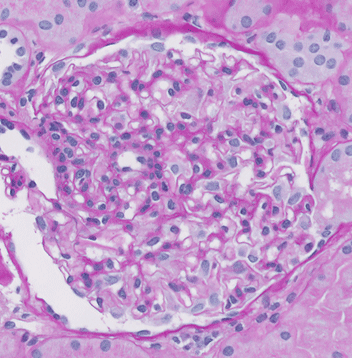
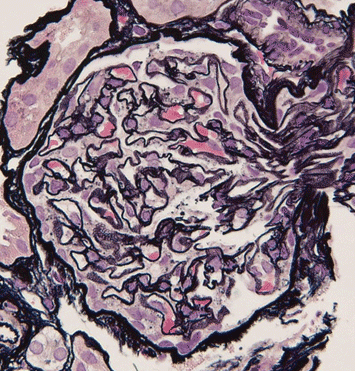
Now, let’s take a look at a couple of pathology slides together
Images courtesy of Dr. Vivel Charu, Assistant Professor of Pathology, Stanford University School of Medicine
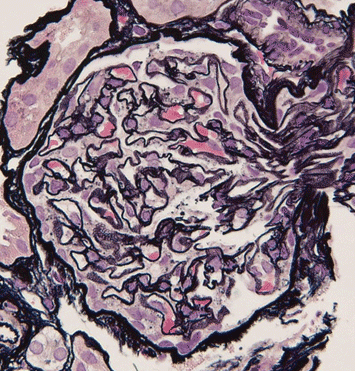
The slide (Jones-silver stain) shows membranous nephropathy. The glomerular basement membrane vacuoles correspond to basement membrane irregularities associated with subepithelial immune-complex deposits seen on the cross-section. In a patient with SLE, the findings would be consistent with Class V lupus nephritis.
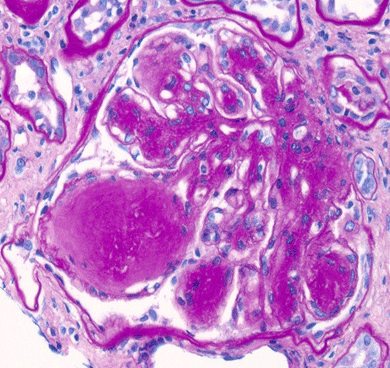
The slide (PAS stained) shows basement membrane thickening and prominent nodular mesangial expansion.
The main differential diagnosis for this light microscopic finding includes:
- Diabetic nephropathy
- Amyloidosis
- Monoclonal Ig deposition disease
- Immunotactoid GN, fibrillary GN
- Idiopathic nodular glomerulosclerosis
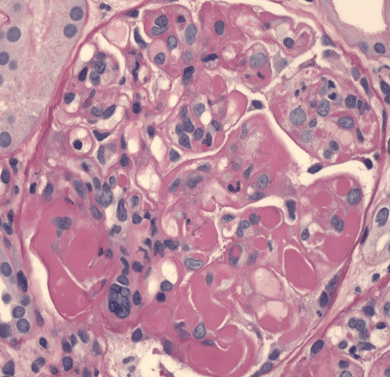
The slide (PAS stained) shows segmental endocapillary proliferation with luminal occlusion by inflammatory cells including numerous monocytes. Several capillary loops are occluded by bulky “hyaline thrombi” (large, subendothelial immune complexes).
The main differential diagnosis for this light microscopic finding includes:
- Cryoglobulinemic glomerulonephritis
- Lupus nephritis (Class IV)

The slide (PAS stained) demonstrates a circumferential cellular/fibrocellular crescent (extracapillary proliferation of >2 layers of cells). The capillary tuft is compressed by the crescent.
The main differential diagnosis for this light microscopic finding includes:
- Pauci-immune necrotizing and crescentic GN (e.g. ANCA-mediated)
- Immune-complex mediated crescentic GN (e.g. IgA, SLE)
- Anti-GBM disease
References:
- Systematic Review and Meta-Analysis of Native Kidney Biopsy Complications by ED Poggio et al. (CJASN Nov 2020, 15 (11) 1595-1602)
- The Renal Biopsy by Patrick D Walker; (Arch Pathol Lab Med. 2009;133:181–188)
- Alian Al-Balas et al. Kidney360 2020;1:797-800