TREATMENT
Pneumocystis Jirovecii Pneumonia Prophylaxis

By Dr. Dilushi Wijayaratne MBBS MD ( Medicine) MRCP(UK)
Honorary Consultant Nephrologist, National Hospital of Sri Lanka
Lecturer in Clinical Medicine
Department of Clinical Medicine
Faculty of Medicine, University of Colombo
Editorial support by: Dr. Paolo Nikolai So, Dr. Mythri Shankar
Pneumocystis jirovecii pneumonia (PJP) is a life-threatening opportunistic infection. It is caused by the ubiquitous fungus, Pneumocystis jirovecii with which the majority of us are infected in early childhood. Latent infection in the lungs may give rise to clinical disease in the immunocompromised. Alternatively, de novo infection contracted by person-to-person transmission or acquired from an environmental reservoir can lead to disease, again on the background of suppressed immunity. While prophylactic antibiotics lower the incidence of PJP in those at risk, the use of these in patients on immunosuppression for glomerular diseases is not standardized.
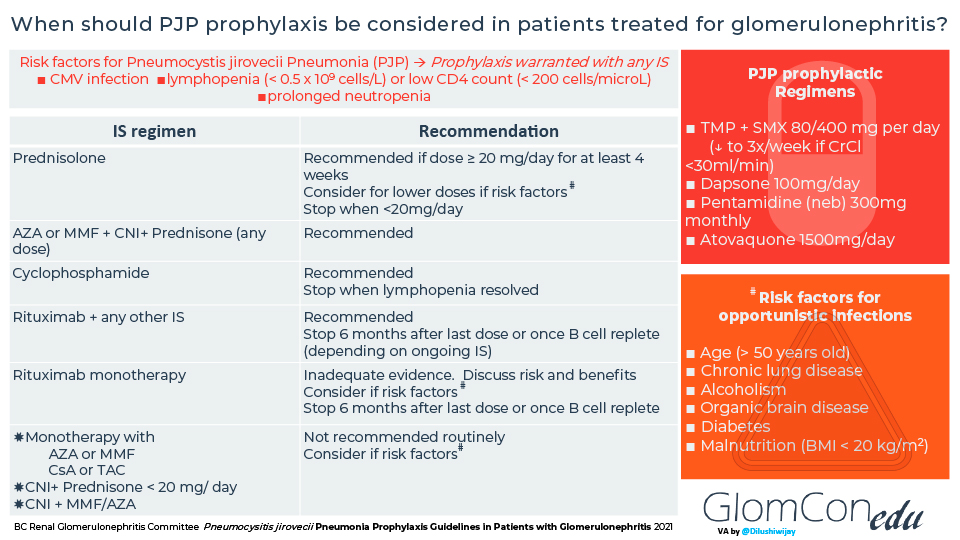
In June 2021, the British Columbia Renal Association published a guideline for PJP prophylaxis in patients on immunosuppression for glomerulonephritis, based on the available literature on the efficacy of PJP prophylaxis in patients on different regimens of immunosuppression. The suggested approach to PJP prophylaxis in patients with glomerulonephritis is presented in this infographic.
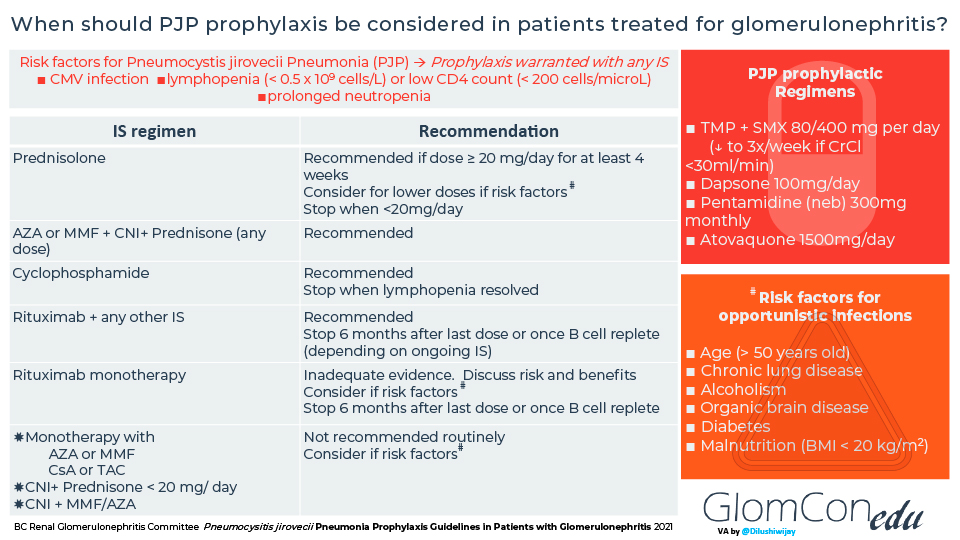
The guideline recommends prevention for patients with certain risk factors based on various clinical scenarios and the immunosuppressive regimen presented in the infographic. Some risk factors bear more weight than others, and clinical judgment is necessary for deciding.
The suggestion is to use PJP prophylaxis in patients with the following risk factors, irrespective of immunosuppressive regimen:
- Cytomegalovirus infection
- Lymphopenia (lymphocyte count < 0.5 x 109 cells/L) or low CD4 count (< 200 cells/microL)
- Prolonged neutropenia
Some authors consider hypogammaglobulinemia a risk factor for PJP. Still, it has not been included in these guidelines because it could lead to over-treatment in patients with nephrotic syndrome.
Trimethoprim/sulfamethoxazole (TMP/SMX) is the first-line drug of choice, based on its higher efficacy than other available prophylactic agents. Alternative agents include dapsone and the relatively more expensive options such as pentamidine (nebulized) and atovaquone.
Further, the recently published KDIGO 2021 guidelines provide general recommendations for PJP prophylaxis for patients on high-dose steroids or receiving cyclophosphamide and rituximab. Specific considerations for each glomerular disease are:
- Lupus nephritis. Consider patients receiving high-dose steroids—however, caution for higher risk of adverse events with sulfa drugs.
- Anti Glomerular Basement Membrane Disease. Consider for the duration of cyclophosphamide therapy.
- ANCA-associated vasculitis. Consider for the duration of cyclophosphamide therapy or six months after the last dose of rituximab (longer for ongoing steroid use).
- IgAN – consider while on prednisolone equivalent ≥0.5 mg/kg/d.
| Drug | Dose | Comments |
|---|---|---|
| Trimethoprim/ sulfamethoxazole |
480mg daily (reduced to 480mg thrice a week if CrCl <30ml/min) | Very effective! InexpensiveImportant adverse effects: GI intolerance; hepatotoxicity; hyperkalemia; Stevens-Johnson syndrome/ toxic epidermal necrolysis (1 per million population per year); photosensitivity; bone marrow suppression |
| Dapsone | 100mg daily | Watch for Haemolytic anemia – may occur with or without G6PD deficiency |
| Pentamidine (Nebulisation) |
300mg monthly | It may be less effective in preventing upper lobe disease
Cautioned in patients with asthma or a smoking history due to risk of bronchospasm -consider pre-treatment with bronchodilator |
| Atovaquone | 1500mg daily | Very expensive! |
References
- BC Renal Glomerulonephritis Committee. Pneumocysitis jirovecii Pneumonia Prophylaxis Guidelines in Patients with Glomerulonephritis 2021
- Kidney Disease Improving Global Outcomes. Clinical Practice Guideline For The Management Of Glomerular Diseases 2021
