OVERVIEW
Basic Principles in Evaluating Glomerular Disease (from The House of Complements)
Acknowledgment: Based on GlomCon’s Glomerular Disease Virtual Fellowship seminar “The Guiding Principles for Evaluation of Glomerular Disorders” by Dr. Richard Glassock., and workshop by Dr. Jessica Lapasia.

Dr. Asta Jonasdottir
Nephrologist
Karolinska University Hospital
Sweden
Measuring Outcomes in Glomerular Diseases: Complete, Partial Remission, Mortality, End-Stage Kidney Disease
How can we assess outcomes such as mortality and end-stage kidney disease in glomerular diseases?
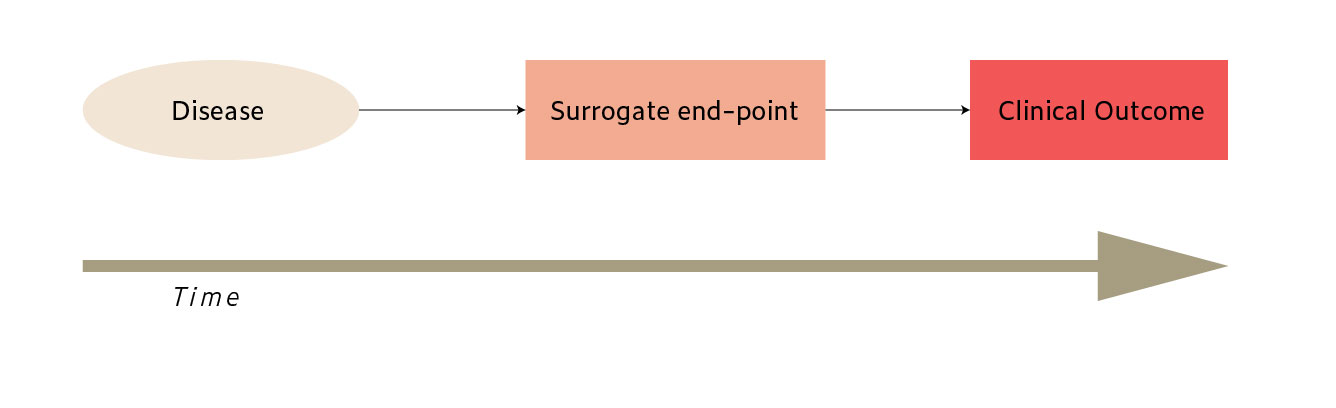
The most definitive clinical outcomes in glomerular diseases are mortality and end-stage kidney disease. However, glomerular diseases are a heterogeneous group of rare diseases with slow progression in many cases. This has led to the use of surrogate endpoints in observational studies and trials. A surrogate-endpoint is a measure that correlates with a clinical endpoint (outcome) and can accurately predict the effects of treatment on the outcome. A change in kidney function is a commonly used surrogate endpoint for ESKD. However, various methods and definitions have been used. Another potential surrogate endpoint is remission, but remission definitions vary between different and even within specific glomerular disease subtypes. Many different disease-specific definitions of remission, such as the absence of systemic disease activity assessed by disease activity measurement tools in multi-organ inflammatory diseases, add additional complexity. This inconsistency in methods and definitions makes it hard to compare study results and treatment effects across studies.
How can we improve outcome measurement and reporting in glomerular diseases?
The Standardized Outcomes in Nephrology (SONG) initiative was started in 2014 to establish standardized core outcome sets for trials in glomerular diseases. Part of the aim is to define outcomes important to glomerular diseases patients and their caregivers, so-called patient-reported outcome measures, which often have been omitted from trials. Although outcomes such as kidney function and mortality are high-ranked among patients and caregivers, outcomes evaluating the quality of life measures are also prioritized.
Drawbacks to Using Proteinuria/Albuminuria as an Endpoint
What are the criteria to apply when assessing surrogate endpoints?
(1) Biological plausibility, (2) epidemiological data, and (3) clinical data.
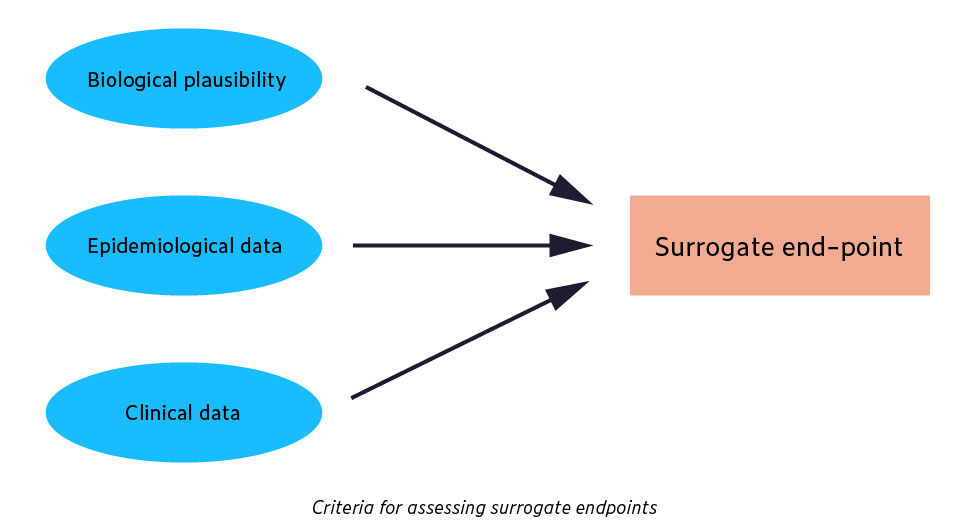
Does proteinuria/albuminuria fulfill the criteria for the surrogate endpoint in glomerular diseases?
Biological plausibility. Biological plausibility refers to whether the surrogate is on a pathophysiological pathway leading to the clinical outcome. Albuminuria/proteinuria may or may not be in the pathophysiological pathway of kidney diseases. Although applicable as a marker of glomerular basement membrane (GBM) function in glomerular diseases, it is not linked to the pathophysiology of certain other kidney diseases such as polycystic kidney disease.
Epidemiological data. Based on the results of a meta-analysis of observational studies, albuminuria was strongly associated with the risk of ESKD in a range of cohorts.
Clinical data. This includes data from randomized controlled trials (RCTs) and makes up the most substantial evidence for surrogacy. There are no large-scale RCTs targeting albuminuria/proteinuria as the primary endpoint, but they have been used as secondary endpoints in many trials. Most of the data come from studies of treatment effects of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers.
Can albuminuria be used as a surrogate endpoint?
A workshop sponsored by the National Kidney Foundation, the US Food and Drug Administration, and the European Medicine Agency analyzed RCTs, observational cohorts, and performed simulations. The results showed a 30% reduction in urine albumin to creatinine ratio (UACR) was associated with a hazard ratio for ESKD of 0.7. However, the group suggests that UACR should only be used for certain conditions, as in diabetic kidney disease with UACR >300mg/g.
Clinical Course and Prognosis of various Glomerular Diseases (indolent, subacute, and rapidly progressive)
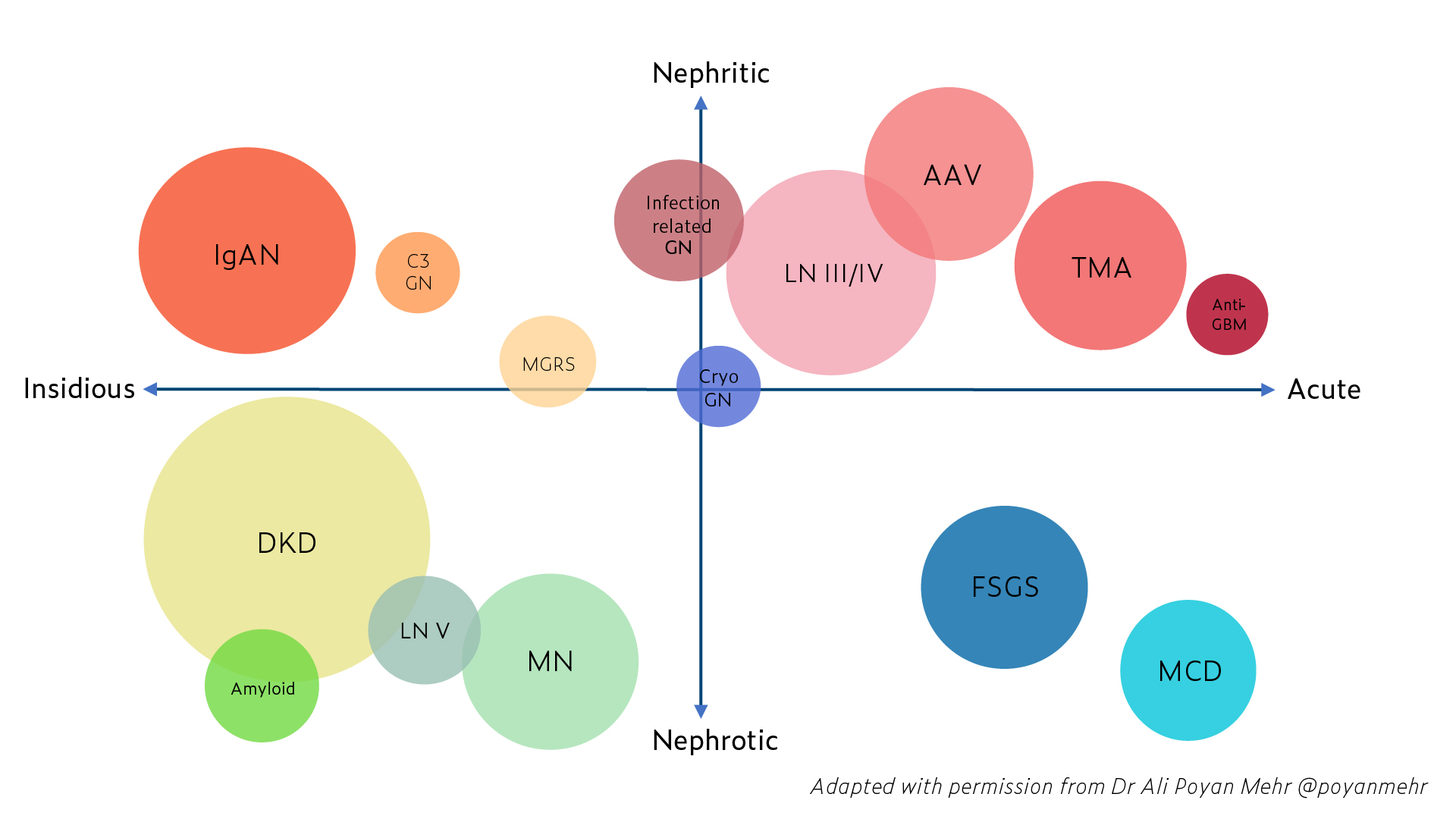
How are the presentation, clinical course, and prognosis of different glomerular diseases?
The presentation of glomerular diseases varies greatly. The figure below shows how different glomerular diseases can present, and some examples are given in the following text.
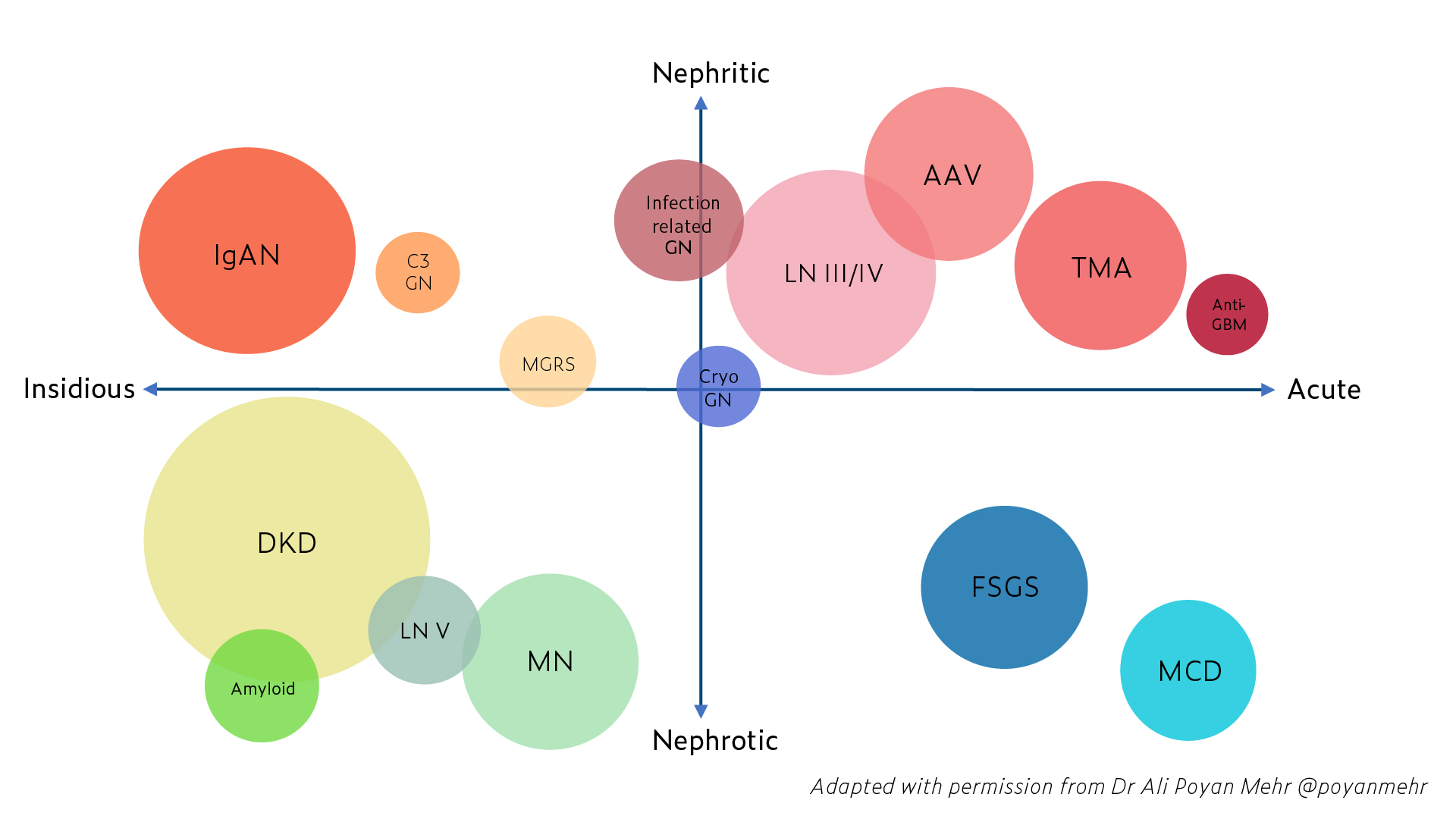
IgA nephropathy: Presentation with recurrent gross or persistent hematuria, proteinuria, or more acutely with crescentic lesions. Around 20-30% of patients progress to ESKD at 20 years.
Membranous nephropathy: Presents with proteinuria and nephrotic syndrome. Five to 30% of patients reach spontaneous remission at 5-year follow-up. If untreated, 14% progress to ESKD at a 5-year follow-up.
Minimal change disease: Typically has an abrupt onset of nephrotic syndrome, proteinuria, and hypertension. Younger age at presentation is associated with a shorter time to complete remission.
Complement 3 glomerulopathies (C3G): Presents with proteinuria, hematuria, +/- low C3 +/- monoclonal gammopathy. The prognosis varies.
Lupus nephritis: Affects around 50% of patients with systemic lupus erythematosus and presents with abnormal urinalysis with or without decreased kidney function. Severity and prognosis vary by class, ability to achieve remission, and the number of relapses.
Vaccination in Glomerular Diseases
Why do we care about vaccinating patients with glomerular diseases?
Infections are among the leading causes of morbidity and mortality in chronic kidney disease patients (CKD). CKD causes immunosuppression, which is multifactorial, a combination of innate and adaptive immune system dysfunction, chronic inflammation, and endothelial cell dysfunction caused by uremia.
What are the current vaccination recommendations for CKD patients?
As summarized in a recently published guide to vaccination, CKD patients should receive routinely recommended vaccinations according to age group and other risk groups depending on their comorbidities. A particular emphasis is placed on three specific vaccines, the hepatitis B (HBV), influenza, and pneumococcal vaccine. However, the true benefit of routine vaccination in this population is not well defined, and more clinical data is needed to determine immunization efficiency. Live-attenuated vaccines are generally considered appropriate if inactivated vaccines are not available, but safety data are limited. However, patients who are receiving immunosuppressive treatment should avoid live-attenuated vaccines.
When should we vaccinate patients with CKD?
Patients with advanced CKD and patients receiving immunosuppressive treatment have a lower rate of seroconversion, lower antibody titers, and less sustained response after immunization than healthy controls. For instance, the HBV vaccine’s response is decreased in advanced kidney disease. This raises the importance of vaccinating CKD patients earlier in the course of the disease.
