NEPHROPATHOLOGY
Obesity-related Glomerulopathy

By Jonathan E. Zuckerman, M.D. Ph.D.
HS Assistant Clinical Professor
Service Chief, Renal Pathology
Director, Surgical Pathology Fellowship
UCLA Department of Pathology and Laboratory Medicine
A representative clinical presentation:
The patient is a 45 year old man with worsening proteinuria that is now ~2g. His past medical history is significant for long-standing hypertension, pre-diabetes, obstructive sleep apnea, and obesity (BMI 36). Serologic workup including ANA, ANCA, SPEP/UPEP, RF, cryocrit, HIV, and hepatitis serologies are negative. His complement levels are normal. His serum creatinine is mildly elevated. A renal biopsy was performed and was significant for the following findings.
Diagnosis:
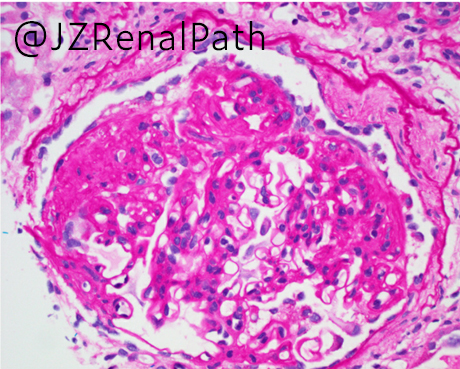
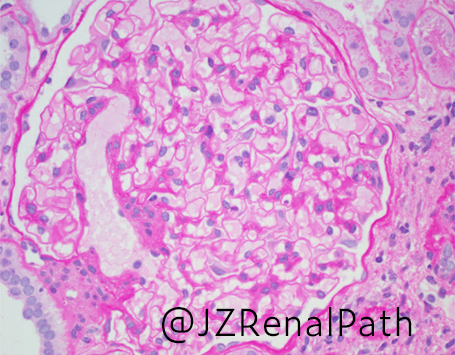
Obesity-related glomerulopathy
Key points:
-
- Defined as glomerulomegaly (glomerular hypertrophy) with or without secondary adaptive segmental glomerulosclerosis arising in obese patients with body mass index >30 kg/m2
- Obesity-associated glomerular hyperfiltration results in prolonged podocyte shear stress with loss of adhesions and detachment ultimately with segmental sclerosis formation
- Similar findings reported in “moderate obesity” (BMI 25-30) suggest some degree of an undetermined genetic component
- Generally presents as slowly progressive proteinuria that may eventually reach nephrotic range but not a true nephrotic syndrome
- Histologic features
- Enlarged glomeruli (>1/2 of a 40x high powered field)
- Thickened GBM
- May see increased mesangial matrix
- Segmental sclerosis, most often a perihilar variant
- Tubular cross-sections enlarged
- Often less interstitial fibrosis/tubular atrophy than other cause of maladaptive glomerular injury
- IF studies are negative (non-specific IgM, C3, and C1q staining of segments of sclerosis may be present)
- EM with patchy partial podocyte foot process effacement (usually ranges from 25-40%)
- Differential diagnoses
- Diabetic nephropathy may show overlapping features and may be indistinguishable. May show hyalinization of both afferent and efferent arterioles
- Primary FSGS will show more extensive podocyte foot process effacement (>75%) and present as true nephrotic syndrome
- Other causes of maladaptive glomerular injury (e.g, renal hypoplasia, obstructive nephropathy, arterionephrosclerosis, etc.)