NEPHROPATHOLOGY
Pauci-immune Glomerulonephritis
In this GlomCon Conference, Dr. Kammi Henriksen shared her expertise with us and reviewed the pathology of pauci-immune glomerulonephritis. Our Moderator’s Notes are derived from her live presentation.

By Dr. Pravir Baxi
Key points:
- Crescentic Glomerulonephritis (GN)
- Histological marker for severe glomerular injury
- Cellular proliferation (> 2 layers of parietal epithelial cells (=podocytes)) and inflammation within Bowman’s space
- Disruption of the glomerular basement membranes (GBM) with fibrinoid necrosis
- Major etiologies include: Immune complex mediated GN, Anti-GBM and Pauci-immune GN
- Histological marker for severe glomerular injury
- Pauci-immune glomerulonephritis (GN) is defined histologically by the presence of necrotizing and crescentic GN with few or no immune deposits on IF or EM
- Most common cause of rapidly progressive GN (RPGN) especially in adults and elderly patients
- 80-90% of pauci-immune GN cases are Anti-neutrophil cytoplasmic antibody (ANCA) positive
- 10-20% are ANCA negative
- Not detected in current assays; IgA ANCAs
- Younger age, fewer extrarenal symptoms, poorer renal survival
- 10-20% are ANCA negative
- ANCA vasculitis
- Autoantibodies (typically IgG class) against lysosomal components of in neutrophils and monocytes
- Specificity for myeloperoxidase (MPO) or proteinase 3 (PR3)
- Pathogenesis
- ANCAs are thought to be pathogenic: neutrophil priming by cytokines (e.g. TNF, C5a) à translocation of cytoplasmic antigens (MPO, PR3) à binding with ANCA Ab à neutrophil activation leading to endothelial injury and complement system activation
- Triggers for ANCA production: environmental (infection and molecular mimicry), genetic predisposition (HLA Class II), defective neutrophil apoptosis, certain drugs
- Drug-induced: propylthiouracil, hydralazine, minocycline, anti-TNF alpha, levamisole
- Idiosyncratic, younger patients, better renal survival, high MPO titers
- Diagnosis of ANCA vasculitis should specify the serotype and clinicopathological variant
- Pathology
- Does not discriminate between various clinicopathology conditions caused by ANCA
- Glomeruli will show fibrinoid necrosis with crescents
- Cellular (days-weeks, potentially reversible), fibrocellular (weeks) and fibrous (weeks-months)
- Vasculature
- Renal vasculitis in 5-35% of cases
- Involves small arteries (interlobular > arcuate), arterioles, capillaries and venules with fibrinoid necrotizing lesions
- Medullary angiitis: inflammation of the medullary vasa recta
- Suggests the presence of systemic vasculitis but is not specific for ANCA GN (i.e. IgAN, cryoglobulinemic GN)
- Granulomatous inflammation: rare in the kidney but seen more in the lung/upper respiratory tract
- Histopathological Classification: allows for uniform reporting, prognostication and guiding treatment
- Focal (> 50% with normal glomeruli, best renal prognosis), Crescentic (> 50% with cellular crescents), Sclerotic (> 50% globally sclerotic, worse renal prognosis)), Mixed (< 50 normal, < 50 crescents, < 50 globally sclerotic)
- ANCA GN can be superimposed/co-existing in other diseases (i.e. LN, anti-GBM)
- Crescents/necrosis out of proportion to immune complex deposition
- Temporal heterogeneity of crescents/level of chronicity (i.e. anti-GBM)
- Autoantibodies (typically IgG class) against lysosomal components of in neutrophils and monocytes
-
- Clinical Aspects
- Granulomatosis with polyangiitis (formerly Wegener’s)
- Necrotizing granulomatous inflammation primarily of lungs and nasal sinuses (saddle-nose deformity)
- Eosinophilic granulomatosis with polyangiitis (previously Churg-Strauss)
- Asthma, peripheral eosinophilia
- Microscopic polyangiitis
- Necrotizing vasculitis mostly affecting multiple sites
- Type of ANCA does NOT permit specific diagnosis but ANCA antigen specificity is associated with disease phenotype/prognosis
- PR3-ANCA: most often granulomatous inflammation, systemic features, higher relapse rate
- MPO-ANCA: most often renal-limited, worse renal prognosis
- Rough correlation of ANCA titers with response and relapse
- 75% will achieve remission but 40% may relapse
- Poor prognostic factors
- Age >65, higher SCr or dialysis dependency at onset, proteinuria, higher chronic histologic indices
- Granulomatosis with polyangiitis (formerly Wegener’s)
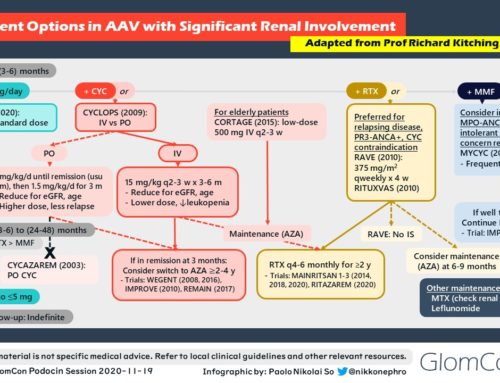
- Treatment options
- Induction: Corticosteroids with Rituximab OR Cyclophosphamide
- Maintenance: Azathioprine OR Rituximab
- Plasmapheresis: can be considered in severe/refractory cases however role may change with upcoming trial data (PEXIVAS)
- Novel therapy under investigation: C5a receptor blockers
- Clinical Aspects
Selected References: