NEPHROPATHOLOGY
The Pathology Lupus Nephritis and Lupus Podocytopathy
A nephropathology conference led by Dr. Isaac E Stillman from Beth Israel Deaconess Medical Center. Our Moderator’s Notes are derived from his live presentation and may include additional information and references which the author and editorial team have included for further reading on this topic.


By. Dr. Harpreet Singh
Key Points:
- Histopathologic lesions that are highly characteristic of LN:
- IgG dominant “full house” glomerular deposits: IgG, IgA, IgM, C1q, and C3
- Glomerular deposits at multiple sites: subendothelial, intramembranous, trans membranous, subendothelial, and mesangial
- Extraglomerular deposits: tubular basement membranes, interstitium, blood vessels
- Prominent tubulo-reticular inclusions/structures
- Mesangial deposits are a prerequisite for the diagnosis of lupus nephritis.
- The original ISN/RPS Classification of Lupus Nephritis (2004) was reviewed and key elements are included here (for the recently revised ISN/RPS classification from February 2018, see a summary at the end)
- Active sediment, proteinuria, nephrotic syndrome, impaired renal function, HTN, anti-dsDNA do not reliably predict lupus class and therefore require a biopsy.
- Class I- Minimal mesangial LN
- normal glomeruli by LM but deposits in the mesangium by IF/EM
- Full house pattern on IF (characteristic in all LN classes)
- minimal clinical renal disease, therefore, these patients rarely undergo biopsy
- Class II- Mesangial Proliferative LN
- Mesangial hypercellularity in association with mesangial immune deposits on IF/EM
- Any subendothelial deposits by LM or capillary wall immune deposits on IF exclude Class II and warrants Class III or IV designation.
- There should be no glomerulosclerosis as a result of pure mesangial deposition. If glomerulosclerosis is seen, then findings are no longer classified as a Class II->. Distinguishing if the glomerulosclerosis is due to LN vs another unrelated issue (aging, hypertension, obesity, etc.) is based on the judgment of the pathologist.
- Clinical correlates: HTN uncommon, < 50% have microscopic hematuria and/or proteinuria (<1 g); Nephrotic syndrome and significant renal insufficiency are very rare and should prompt a search for another cause (eg. Podocytopathy).
- Class III- Focal proliferative LN
- <50% of glomeruli have evidence of glomerular lesion (proliferation, necrosis, “wire loops”, Karyorrhexis, crescents) involvement by LM, although other glomeruli might have Class II mesangial lesions
- If the proliferation is very focal or the sample size is small, it may be misleading and lead to under calling the biopsy findings as a Class II LN.
- Combined Class III (or IV) and Class V requires extensive sub-epithelial deposits (in addition to the subendothelial deposits that characterize Class III/IV LN), defined as at least 50% of the glomerular capillary surface of at least 50% of glomeruli by LM or IF.
- Clinical correlates: variable, 1/3rd with HTN, hematuria/proteinuria in about 50%, decreased GFR in 25%, and nephrotic syndrome in about one 3rd
- Class IV- Diffuse Proliferative LN
- >50% of glomeruli by LM
- Most common class seen (likely result of who clinicians decide to biopsy)
- Previously classified into segmental, IV-S or global, IV-G
- IV-S: >50% of involved gloms have segmental lesions; IV-G: >50% of the involved gloms have global lesions
- Controversy about whether the subdivision of class IV into segmental and global should continue exists [This is suggested to be eliminated in the new ISN/RPS classification from February 2018, see below]- historically evidence suggested that IV-S did worse clinically than IV-G
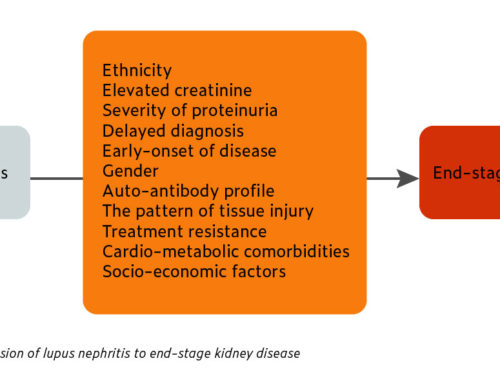
- Clinical correlates: hematuria and proteinuria are present in virtually all patients, frequent nephrotic range proteinuria (~50%), HTN, reduced eGFR, hypocomplementemia (esp C3), elevated anti dsDNA levels
- Class V- Membranous LN
- Global or segmental continuous granular subepithelial immune deposits, often with concomitant mesangial deposits/hypercellularity
- Scattered subendothelial deposits may be identified by IF or EM; if visible by LM, warrant a combined Class III or IV depending on the distribution.
- Clinical correlates: nephrotic syndrome, similar to idiopathic membranous nephropathy; microscopic hematuria and HTN may also be seen; sCr usually only slightly elevated or normal; up to one 3rd may present without extra-renal disease; may precede the diagnosis of SLE by months or years; may present with no other clinical or serologic manifestations of SLE (serologic markers may be negative)
- Class VI- Advanced sclerosis LN
- At least 90% global glomerulosclerosis with clinical or pathologic evidence that the sclerosis is attributable to LN (can be challenging to determine)
- No evidence of ongoing active glomerular disease; usually marked IFTA
- NIH Activity vs. Chronicity Index
- Can be more helpful with regards to treatment decisions; debate about reproducibility; present in new 2018 classification (see below).
- Activity index parameters (graded 0-3, total score 0-24): endocapillary hypercellularity, glomerular neutrophils, karyorrhexis/fibrinoid necrosis (x2), cellular crescents (x2), hyaline deposits (thrombi/wire loops), interstitial inflammation
- Chronicity index parameters (graded 0-3, total score 0-12): glomerular sclerosis, fibrous crescents, tubular atrophy, interstitial fibrosis
- Activity index >11 or Chronicity index >3 -> high risk of ESRD
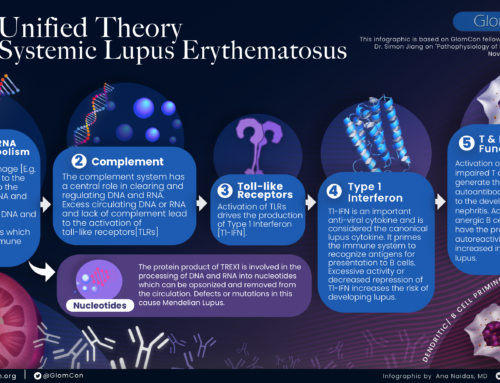
- Nonimmune complex Injury in SLE
- ANCA
- Consider if scant immune complex deposits but fibrinoid necrosis and crescents.
- Always check an ANCA when the necrotizing, crescentic disease is noted on biopsy.
- Podocytopathies
- Can see Class II lesions on LM and on EM, but with massive podocyte effacement.
- MCD or FSGS patterns of injury
- Very difficult to diagnose MCD in addition to Class III, IV, V, as these can already be associated with podocyte effacement and proteinuria (esp. Class V)
- Antiphospholipid or cryoglobulin autoantibodies may promote thrombotic and inflammatory vascular lesions
- Lupus vasculopathy- characterized by necrosis and IC that occlude the lumen of arterioles and small arteries, bad prognostic sign (seen esp in Class III and IV) (Gonzalez-Suarez ML, Lupus 2014)
It is important to note that the classification of the pathology of lupus nephritis has been subject to major modification as outlined by the ISN/RPS Working Group for lupus nephritis in their Phase 1 report in February 2018 (https://www.kidney-international.org/article/S0085-2538(17)30859-1/pdf 6). Key highlights from this report include:
- Reassessment of the threshold for what would be considered mesangial hypercellularity in class II lupus nephritis
- Elimination of the term “endocapillary proliferation” in favor of “endocapillary hypercellularity” to better reflect the nature of underlying pathology.
- A lower threshold to what degree of extracapillary proliferation would be considered “crescents” and the explicit inclusion of fibrin and fibrous matrix as components of the crescents.
- Detailed definition of cellular versus fibrous versus fibrocellular crescents
- A formal definition for what defines fibrinoid necrosis: “fibrin associated with glomerular basement membrane disruption and/or lysis of the mesangial matrix; this lesion does not require the presence of karyorrhexis”
- Elimination of segmental and global subdivision of class IV due to the lack of interobserver agreement and unclear clinical significance
- Elimination of the current dichotomous activity/chronicity designation (A, C, A/C) in favor of a more nuanced and quantitative grading through a modified NIH lupus nephritis activity/chronicity scoring system
- Inclusion of the tubulointerstitium as a compartment for assessment of inflammation and fibrosis